
Meru Sheel, Australian National University; Cyra Patel, Australian National University, and Margie Danchin, Murdoch Children’s Research Institute
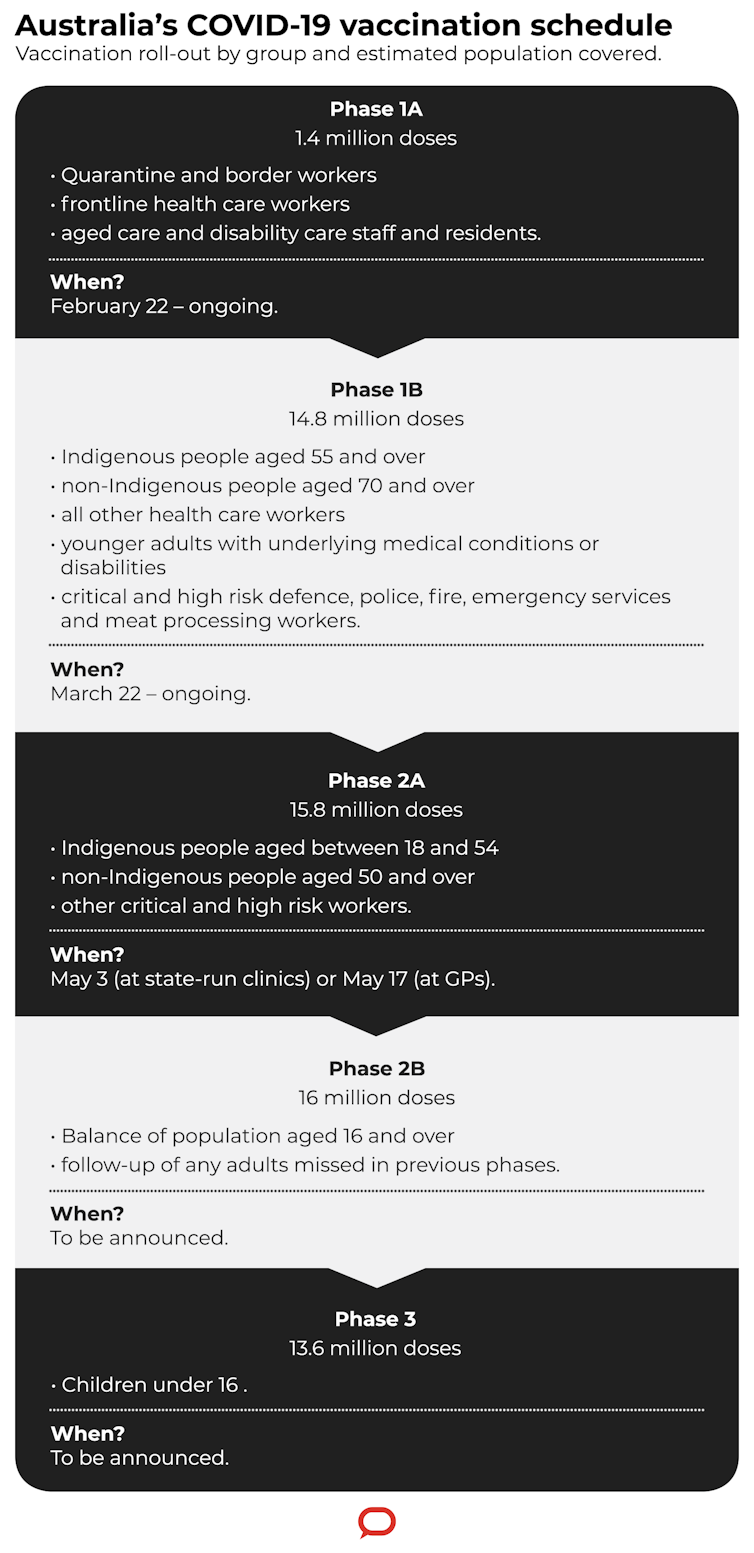
From today, Australians aged 50 or older are eligible to receive their COVID-19 vaccine from special respiratory clinics or mass vaccination hubs in some states. Appointments with selected GPs are available from May 17.
However, a recent poll shows many people over 50 are hesitant to get vaccinated, particularly with the AstraZeneca vaccine earmarked for them. That’s mostly due to reports of very rare, but serious, blood clots that can develop after vaccination.
So it’s understandable why people want to know about any safety issues and how they relate to age. It’s also natural to want to know how well the vaccine works to protect people over 50.
Here’s what we know about this safe and effective vaccine from clinical trials and around 136 countries using it so far.
Clinical trials, which have included more than 57,000 people to date, found the AstraZeneca vaccine to be safe and effective.
When researchers pooled the results from four large trials — including about 8,600 vaccinated people and a similar number of unvaccinated persons — there were 81% fewer COVID-19 cases in vaccinated people than in unvaccinated ones. No one who got the vaccine was hospitalised due to COVID-19.
While the studies haven’t been designed specifically to look at efficacy in distinct age groups yet, there is good evidence the AstraZeneca vaccine protects both the elderly and younger adults from COVID-19. In clinical trials, adults aged 18-55 and those older than 55 had similar immune responses.
How about serious disease and death?
When it comes to protecting people from serious disease, there’s good news again. We have data from England and Scotland that one dose of it reduces COVID-19 hospitalisations by 80-88% in the elderly, similar to that of the Pfizer vaccine (88-91%).
Based on our understanding of how vaccines work — generally, vaccines are more effective in younger adults — it’s safe to assume the vaccine is at least 80% effective in preventing severe COVID-19 in people over 50.

What about the new variants?
New variants of SARS-CoV-2, the virus that causes COVID-19, affect the efficacy of the AstraZeneca vaccine, but only slightly for the B.1.1.7 strain (the UK variant). It’s about 70% effective against this strain, compared with about 82% for the original strain.
However, there have been some concerns about protection against the B.1.351 strain (the South African variant). This is because the AstraZeneca vaccine provides less protection against mild COVID-19 disease in people infected with it.
Does the AstraZeneca vaccine limit spread of COVID-19?
We still need more long-term data to say for certain whether the vaccine prevents transmission of COVID-19.
However, preliminary UK research provides some welcome news. Researchers looked at more than 365,000 households and nearly one million contacts of COVID-19 cases. They found the vaccine reduced transmission from people vaccinated with one dose by 40-50%. This is great news in terms of slowing the spread of the disease.
Both clinical trials and real-world data confirm the AstraZeneca vaccine has a good safety profile similar to other vaccines commonly used in Australia.
Side-effects are common and are mostly mild to moderate, with few recipients needing medical attention. The most common are reactions at the injection site, fatigue, headache and muscle pain. These occur in half to three-quarters of people under 55 after their first dose, and are less common in older people. The side-effects generally start within 24 hours and last around one or two days, and indicate your immune system is working.
In Australia, data from the AusVaxSafety vaccine surveillance system shows about 22% of people vaccinated with the AstraZeneca vaccine missed a day or more of work or studies as they were unwell. Fewer than 2% needed to see a doctor.
Read more:
COVID vaccines have been developed in record time. But how will we know they’re safe?
Serious reactions to the vaccine have been very rare, one of which includes thrombosis with thrombocytopenia syndrome, which is on everyone’s mind right now.
This is a very rare condition in which blood clots (thrombosis) and low levels of platelets (thrombocytopenia) occur 4-28 days after receiving the vaccine. This can lead to disability and 20-25% of people with these clots die.
About six in every million people vaccinated with the AstraZeneca vaccine develop the condition. And it tends to be more common in people under 50. Other than younger age, there are no other risk factors for these clots we know of yet.
In Australia, there have been six cases of this type of blood clotting: one person in their 30s, four in their 40s, and one in their 80s. Of these, a person in their 40s has died from it.
Read more:
What is thrombocytopenia, the rare blood condition possibly linked to the AstraZeneca vaccine?
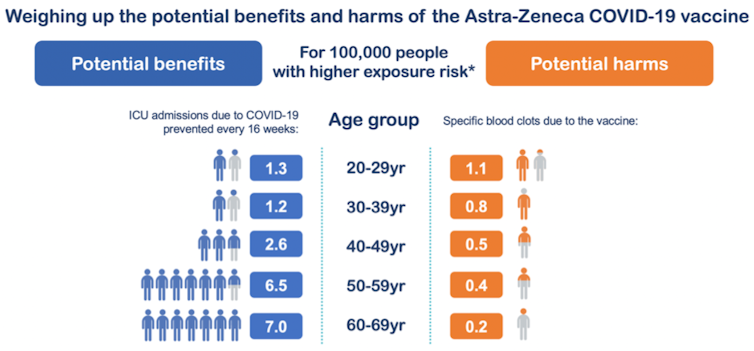
The risk-benefit analysis for Australians right now differs depending on the amount of COVID-19 in the community, your age and the availability of alternative vaccines.
Based on a small amount of data so far, the risk of these blood clots after the AstraZeneca vaccine, for people aged 50-59 is about 0.4 per 100,000 and for those aged 60-69, 0.2 per 100,000.
But the risk of getting severe COVID-19 or the risk of admission into intensive care from COVID-19 is much higher for the over 50s — nearly ten-fold higher than the risk of clots after the vaccine.
It’s about 6.5 per 100,000 people aged 50-59 and 7.0 per 100,000 for people aged 60-69, based on data from Victoria’s second wave in July 2020. There are different risk-benefit calculations for different scenarios.
Australia has almost no disease in the community. However, this could change very quickly if there were new outbreaks. We also have no alternative to the AstraZeneca vaccine for most people over 50 (more Pfizer vaccine is not available until the last quarter of 2021). So balancing the risks and benefits of the vaccine, is extremely challenging. People may not perceive their risk of COVID-19 as high enough to warrant vaccination and are preferring to wait, perhaps six months or more until other vaccines are available.
However, the potential benefits of the vaccine go far beyond what we’ve already mentioned. Vaccination will contribute to the prevention of long COVID-19 (symptoms that linger for months) as well as increased ability to move around freely in society, including being able to attend large events. Vaccination will help us avoid lockdowns or school closures, allow us to travel overseas and return to normal life.
Read more:
A balancing act between benefits and risks: making sense of the latest vaccine news
You can use the government’s vaccine eligibility tracker to check whether you can receive your COVID-19 vaccine from today, and to make an appointment.
This will give you details of the state- and territory-run vaccination clinics near you that are open from today (not all are taking appointments for the over 50s yet). From May 17, you can receive your vaccine at some GP clinics.
Two doses of the AstraZeneca vaccine are needed for best protection, preferably 12 weeks apart.
Meru Sheel, Epidemiologist | Senior Research Fellow, Australian National University; Cyra Patel, PhD candidate, Australian National University, and Margie Danchin, Paediatrician at the Royal Childrens Hospital and Associate Professor and Clinician Scientist, University of Melbourne and MCRI, Murdoch Children’s Research Institute
This article is republished from The Conversation under a Creative Commons license. Read the original article.
IMPORTANT LEGAL INFO This article is of a general nature and FYI only, because it doesn’t take into account your personal health requirements or existing medical conditions. That means it’s not personalised health advice and shouldn’t be relied upon as if it is. Before making a health-related decision, you should work out if the info is appropriate for your situation and get professional medical advice.